Inoculating the Public: Managing Vaccine Rhetoric
This past year, the onset of North America’s flu season coincided with reporting on a novel turn in the ongoing effort to fend off contagion: the use of social media to coordinate “pox parties” and to market mail-order lollipops “infected” with chicken pox to parents planning to expose their children to the live virus.1 The reasoning behind these practices, that helping children develop “natural immunity” would be less harmful than exposing them to the varicella (chicken pox) vaccine, positioned this emerging issue as a development in the anti-vaccination movement, a movement motivated by the discredited link between autism and the measles, mumps, and rubella (MMR) vaccine first proposed by Dr. Andrew Wakefield in the early nineties. In challenging the effectiveness and safety of childhood vaccination, vaccine opponents weaken public confidence in immunization programs such as MMR. Vaccine proponents therefore often counter that, by framing immunization as if it is, first and foremost, a matter of personal opinion, vaccine debate itself risks intensifying the anti-vaccination movement and undermining one of our most effective defenses against contagion.2 Indeed, whether news reports accurately reflect growing health trends, attention paid by the media to unconventional alternatives to vaccination would seem to encourage the persistence of the vaccine debate.
In raising questions about the relationship between scientific knowledge, health beliefs, and public-health policy and practice, the vaccine debate presents an opportunity to consider what part persuasion plays in the management of public health. In this article, I argue that contemporary public health campaigns characterize rhetoric itself as corrective, a method of managing the health of the group through the isolation of harmful attitudes and beliefs. My aim is not simply to displace this view but to understand it in relation to contemporary social and epistemological shifts, such as the use of the web to circulate information about public-health emergencies. From there, I critique the ability of public health campaigns based on a sense of rhetoric as corrective to adequately counter anti-vaccination. In particular, I take up one of the most pervasive rhetorical strategies for constituting, and countering, the two sides to the vaccine issue, the commonplace that holds there to be “facts and fictions” or “myths” of science. I consider this strategy in light of a cornerstone of contemporary public health, scientia potentia est, or “knowledge is power,” a premise that often underlies and structures public health policy and practice, sometimes in implicitly disempowering ways.3
Public Misunderstanding of Science, Anti-Vaccination, and the “Age of Credulity”
At the end of this past summer, Ottawa Citizen science reporter Tom Spears bemoaned the “age of credulity” in which we live, “a constant state of disbelief where, despite having more education than any society in human history, people would rather take the word of an anonymous Internet post over that of a recognized authority, especially where there’s a conspiracy theory” (A1). The hallmark of this age, as Spears elaborates, is the public misunderstanding of science, the worst symptom of which is the anti-vaccination movement because it can be linked to recent outbreaks of measles and, more problematically, the spread of “claims that H1N1 vaccine will kill you” (A1). Spears is one voice in a bigger debate over how the scientific community can adapt the burden of proof in the face of communication technologies that remediate, reframe, and recirculate their research faster and farther than ever before, as well as in response to social movements, such as anti-vaccination, that threaten to undo the triumphs over infectious disease that marked the mid-twentieth century.
Recently, for example, a group of psychologists from Cardiff University argued in a Guardian op-ed that scientists should “be allowed to check stories on their work before publication” on the grounds that “public trust in science, and in science reporting, is harmed far more by inaccuracy than by non-independence” (Sumner, Boy, and Chambers n. p.). This was a response to Ananyo Bhattacharya, the online editor of Nature, who two weeks earlier had argued that copy checking should be prohibited because “scientists have a vested interest in the way their work is portrayed in the media” (n. p.)—not least of which is funding. During that same month, however, while being interviewed for the podcast, “This Week in Virology,” medical writer Trine Tsouderos argued in support of copy checking by describing science journalism as akin to a non-native speaker presenting Chinese to a fluent audience, and characterizing science as a “grammar” that needed to be corrected by an expert whenever it was moved from the scientific community into the media.
Tsouderos’s discussion of fact-checking prompted this response from co-host and molecular biologist Rich Condit: “Wow, I hope there’s a whole bunch of people listening, okay? . . . ’cause this is important stuff, that’s great” (Racaniello and Despommier n. p.). That this discussion took place on a “podcast about viruses—the kind that make you sick” served as a reminder that the vaccine wars have unfolded against the backdrop of ongoing apprehension over how scientific knowledge is reported to the public. While much of this discussion has centered on the possibility of allowing scientists more control over how their research is conveyed, the suggestion that scientific knowledge, when abstracted from its original context, may be harmful to the public has been made much more persuasive by the attribution of the return of preventable childhood infections such as measles to a rise in unfounded beliefs about vaccine science, rather than to other issues that have gained greater attention in the past year, such as the growing wage gap in North America and inadequate access to health care. In other words, while it’s critical that correlation does not equal causation in the context of vaccine science, the same principle is often moot in assessments of vaccine rhetoric.
Flu Facts, Flu Fictions
Preoccupation with the harmfulness of vaccine rhetoric took on new exigency more than two years ago, when the World Health Organization (WHO) declared H1N1 a Phase Six pandemic alert and North Americans were faced with immunization on a massive scale. In October 2009, science advocate and vaccine developer Paul Offit voiced emphatic concern over how vaccine skepticism would affect Americans’ ability to cope with H1N1. In a New York Times op-ed titled “Nothing to Fear but the Flu Itself,” Offit characterized anti-vaccination as both a health risk and a strain on public resources, observing that “[p]ublic officials [were then] battling not only a fast-spreading influenza virus but also unfounded fears about the vaccine that can prevent it” (n. p.). Offit then raised, and quickly dismissed, four beliefs about the H1N1 vaccine, most of which apply to anti-vaccination in a broader sense: first, that it was unsafe; second, that it was untested; third, that it contained a dangerous adjuvant; and fourth, that it had a dangerous preservative. These beliefs were “myths,” according to Offit, and he added that they were underwritten by the more insidious belief that “Americans have more to fear from the vaccine than the deadly disease it prevents.” Vaccine myths, which were circulating, unchecked, via “TV talk shows and the Web,” would make it harder for frontline health workers to distribute vaccine to those who need it most (n. p.).
The point of the op-ed was not to encourage vaccination by motivating sympathy for health professionals, however. Apart from the pathos characteristic of the op-ed genre, Offit’s appeal was made on the grounds that beliefs themselves can be harmful to your health. As Offit puts it at the close of his piece,
New myths will inevitably arise as some of the millions of people who are inoculated against H1N1 flu suffer unrelated illnesses . . . . One can only hope that the American public will understand that subsequence isn’t necessarily consequence, and not be scared away from a vaccine that can save lives. (n. p.)
Offit thus tackled the health risk of anti-vaccination beliefs by reinforcing the boundary between the facts and fictions of vaccine science—the boundary between “good” knowledge and “bad” belief—in a move that is exemplary of the most pervasive rhetorical strategy adopted by public health agencies to encourage individuals to get the H1N1 vaccine. This strategy, which has a kinship with the commonplace of knowledge as power, continues on in the present-day promotion of the annual flu vaccine.
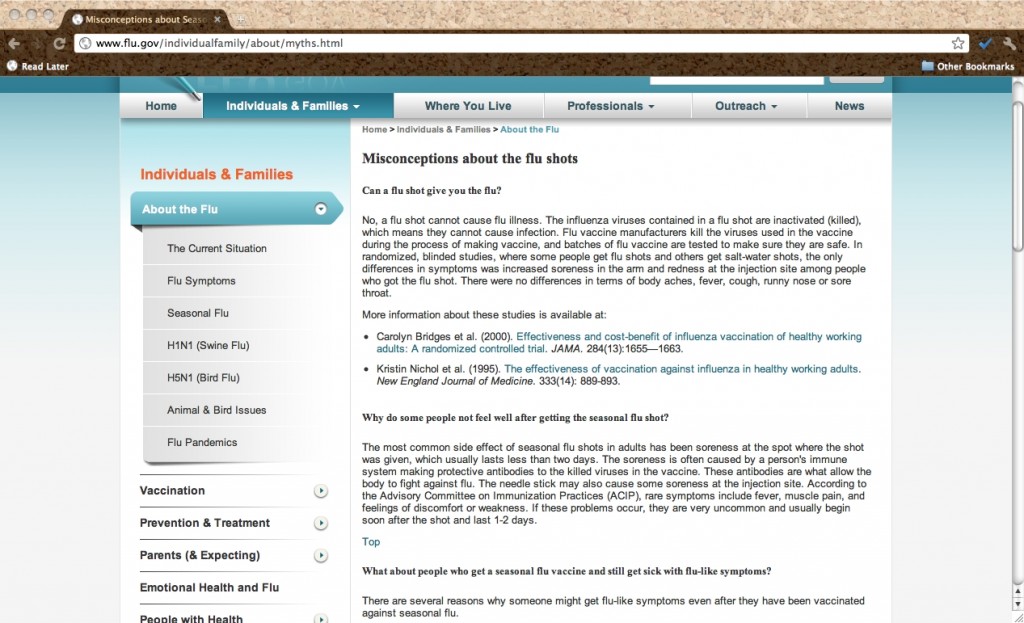
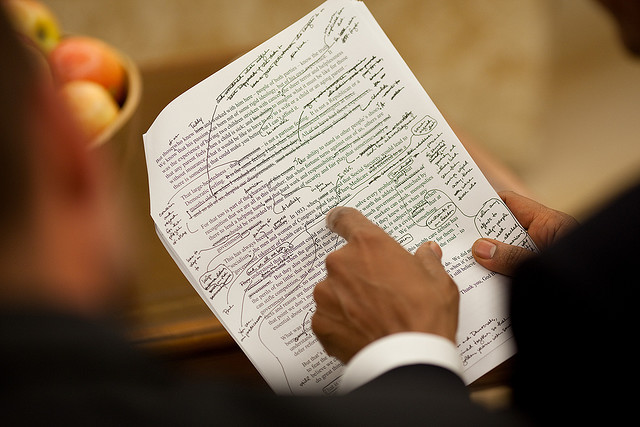
On the U.S. website Flu.gov, for example, information about the flu vaccine is provided under the heading, “Misconceptions about Seasonal Influenza and Influenza Vaccines” (see Figure 1). Whoever encoded this material for the web named the file “Myths.html” in a move suggestive of the pervasiveness of this conception of vaccine rhetoric. The discussion of everything from the timing to the potential side effects of flu shots is here presented as if hesitation to vaccinate is always irrevocably the result of misunderstanding, a lack of proper knowledge that can be remedied through targeted corrective. Little else is said about what other reasons might prohibit individuals and families from being vaccinated—financial limitations, time management and childcare needs, lack of continuity of healthcare—not to mention how they might be supported by the agency in overcoming such obstacles.
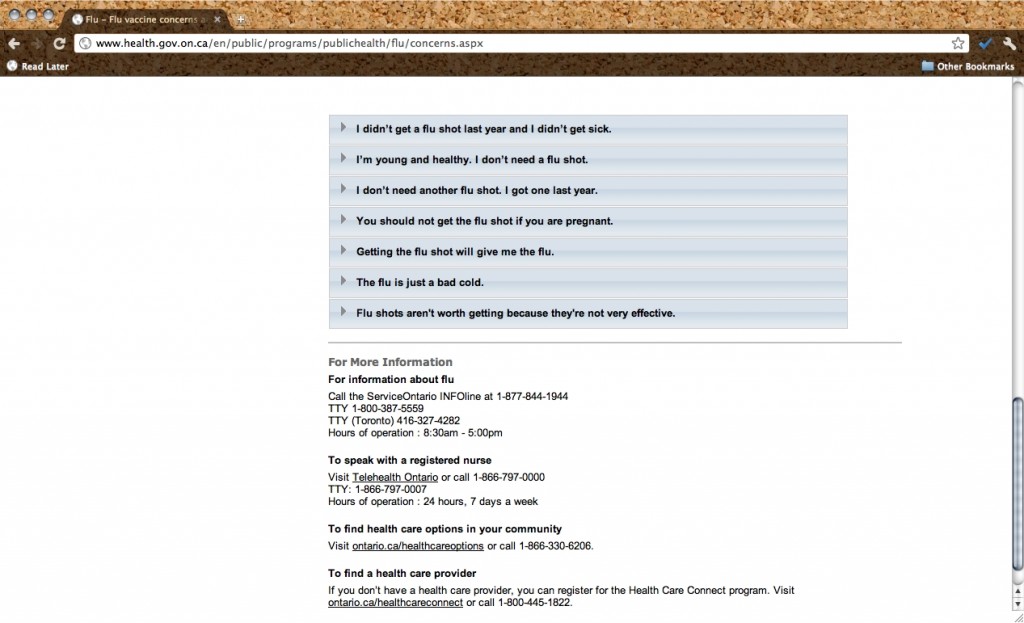
Ontario’s Ministry of Health and Long-Term Care also continues to provide information by enumerating seven “myths” of the flu virus, from “I don’t need another flu shot. I got one last year” to “I’m young and healthy. I don’t need a flu shot” (“Flu Virus,” n. p., see Figure 2). Tension between the sense of these reasons as myths, on the one hand, and excuses, on the other, perhaps marks the point at which the rhetorical management of vaccine skepticism as a matter of the public’s misunderstanding of science begins to break down.
Even when the language of fact and fiction is conspicuously absent from web-based North American flu shot campaigns, information is still conveyed online by way of “Frequently Asked Questions,” a format not unique to public health but nevertheless suggestive of asymmetry between what an individual user believes and what is actually true. Nearly every page of the Public Health Agency of Canada’s website gives information about H1N1 and influenza via question and answer. One question, however, reads, “Why does your information about H1N1 keep changing?” (“Frequently Asked Questions – H1N1 Flu Virus,” n. p.). (This was, in fact, my question when I noticed how many updates had been made to the Public Health Agency’s H1N1 page in early 2011, well after the pandemic had been declared over.) It is the only question on a national public health web page that even remotely addresses a potential cause for confusion over vaccination besides misunderstanding.
If it is the case that North Americans make decisions about vaccination not only by consulting public health campaigns but also by engaging in the vaccine debate, then it is possible that the uptake of the H1N1 vaccine was stymied by the reliance, on both sides of the controversy, of the same grounds for urging North Americans to decide either in favor of or against getting the shot.4 In vaccine public discourse, getting it and not getting it were both strenuously represented as posing potentially serious health risks. On one hand, the vaccine, especially the vaccine with an adjuvant, was represented as a health risk that could, at the very least, cause swine flu, and, at the worst, induce paralysis or death. On the other hand, an anti-vaccine stance was frequently portrayed as a potentially bigger risk because it could jeopardize the health of the individual and the group. And these individuals would not only be spreading swine flu; they would also be spreading a “panic virus” that could induce a kind of intellectual paralysis among those who might otherwise opt for inoculation.
Better Living through Rhetoric
Because it allows us to hypothesize a link between specific lines of public-health argument and the empirical outcomes of epidemic, rhetorical analysis may be, like fact-checking, a relevant method of correcting misunderstanding, one that could lead to the development of better public health campaigns: that is, rhetoricians can offer right arguments for seeking the vaccine, and can point out exactly where public health is failing the public. Yet, rhetoricians of health and medicine can also challenge and critique the effectiveness of the instrumental view of persuasion entailed by the commonplaces that regulate public health, such as that knowledge is power and that fact is knowledge, while belief is fiction. These simple constructions compete with an equally problematic view of persuasion suggested by a metaphor that dominates the broader public debate over vaccination: the metaphor of vaccine rhetoric as itself an epidemic. The metaphor of anti-vaccination belief as an epidemic is a particularly virulent one, inversely related to the view of knowledge as an inoculation. The ubiquity of this novel subtype of the broader metaphor of beliefs and ideas as epidemics is itself ironic considering the predicament we find ourselves in, as vaccination rates drop and previously eliminated contagions make their return. That is, why frame public-health knowledge—which is, in a word, public-health power—as an inoculation at a moment when vaccination rates have apparently hit a record low? The epidemic metaphor frames belief as itself potentially deadly, to be combated through simple rhetorical intervention. Yet belief is not something we could do without if we want individuals to accept vaccine science, nor is it mutually exclusive from knowledge.
Vaccines have afforded us some control over communicable disease, making it that much easier to cope with contagion and, by extension, with life in the group. Out of that control extended a reasonably clear chain of command over a critical area of public health. In that context, knowledge was power because it meant knowing medicine could treat devastations that formerly fell under the purview of morality. Now, however, as suggested by discussions, in expert, professional, and public arenas, on how to manage vaccine rhetoric for the sake of our health, the stakes of scientific knowledge have changed. Rhetorical analysis might support the development of better public health campaigns. However, as rhetoricians, we might, in lending to this effort, apply ourselves toward further examination of the motivations of these same campaigns, such as the notion that they can be used to effectively inoculate the public against scientific misconceptions. Knowledge isn’t the same thing it was in the early years of microbiology, nor is health. Stepping back to think about vaccine skepticism differently might both improve vaccination rates and fend off a return of deadly illness. Communicable disease is a human problem—and it is a global problem. In that context, treatment, not knowledge, is power.
Endnotes
- See, e.g., “Parents Warned About Mail Order Chicken Pox Lollipops,” (Tanglao).return
- Many proponents see vaccine debate as a manufactured scientific controversy. “A scientific controversy is ‘manufactured’ in the public sphere,” writes rhetorician Leah Ceccarelli, “when an arguer announces that there is ongoing scientific debate in the technical sphere about a matter for which there is actually an overwhelming scientific consensus” (196). The purpose of the manufactured scientific controversy is to promote or delay public policy, but another effect of the will to debate motivated by this rhetorical strategy is the sense that “agreement to debate is taken by audiences to indicate that there are two equally strong sides on the matter within the scientific community” (198). In his account of MMR vaccine controversy, The Panic Virus, journalist Seth Mnookin discusses the use of what Ceccarelli calls “the fairness appeal” (198) to gain air time for the views of the anti-vaccination movement. Under this appeal, debate is permitted as a result of “needing to be fair to those on ‘both sides’ of an issue about which there was nothing up for debate—at least not in the real world” (Mnookin 9).return
- For a more detailed discussion of the knowledge enthymeme in public health, see Blake Scott’s Risky Rhetoric.return
- Health Canada, for example, reported in 2010 that four in 10 Canadians opted to get the H1N1 vaccine (see “H1N1 Shots Skipped by 60% of Canadians”).return
Works Cited
- Bhattacharya, Ananyo. “Scientists Should Not Be Allowed to Copy-Check Stories about their Work.” The Guardian, 29 Sept. 2011. Web. 27 Oct. 2011.
- Ceccarelli, Leah. “Manufactured Scientific Controversy: Science, Rhetoric, and Public Debate.” Rhetoric & Public Affairs 14.2 (2011): 195-228. Print.
- “Flu Virus.” Health.gov.on.ca. Ontario Ministry of Health and Long-Term Care, 30 Nov. 2010. Web. 1 Nov. 2011.
- “Frequently Asked Questions – H1N1 Flu Virus.” FightFlu.ca. The Public Health Agency of Canada, 28 Sept. 2010. Web. 27 Oct. 2011.
- “H1N1 Shots Skipped by 60% of Canadians.” CBCNews Health, 30 Sept. 2010. Web. 15 Nov. 2011.
- “Misconceptions About Seasonal Influenza and Influenza Vaccines.” Flu.gov. Flu.gov, 8 Sept. 2011. Web. 27 Oct. 2011.
- Mnookin, Seth. The Panic Virus: A True Story of Medicine, Science, and Fear. New York: Simon & Schuster, 2011. Print.
- Offit, Paul A. “Nothing to Fear but the Flu Itself.” The New York Times, 11 Oct. 2009. Web. 27 Oct. 2011.
- Racaniello, Vincent, and Dick Despommier. “Live at ICAAC in the Windy City.” This Week in Virology, 18 Sept. 2011. Web. 27 Oct. 2011.
- Scott, J. Blake. Risky Rhetoric: AIDS and the Cultural Practices of HIV Testing. Carbondale, IL: Southern Illinois University Press, 2006. Print.
- Spears, Tom. “The Age of Credulity.” The Ottawa Citizen 7 July 2011: A1. Print.
- Sumner, Petroc, Frederic Boy, and Chris Chambers. “Scientists Should Be Allowed to Check Stories on their Work Before Publication.” The Guardian, 11 Oct. 2011. Web. 27 Oct. 2011.
- Tanglao, Leezel. “Parents Warned About Mail Order Chicken Pox Lollipops.” ABC News, 6 Nov. 2011. Web. 6 Nov. 2011.


 Monica Brown is a PhD candidate in the Department of English at the University of British Columbia in Vancouver, Canada, where she specializes in rhetoric of health and medicine. Her dissertation research investigates the influence of risk discourse on public-health promotion during a global pandemic. She also researches metaphor and medicalization. Her chapter, “Woman as Mysterious Machine,” appeared in The Tapestry of Health, Illness, and Disease (2009).
Monica Brown is a PhD candidate in the Department of English at the University of British Columbia in Vancouver, Canada, where she specializes in rhetoric of health and medicine. Her dissertation research investigates the influence of risk discourse on public-health promotion during a global pandemic. She also researches metaphor and medicalization. Her chapter, “Woman as Mysterious Machine,” appeared in The Tapestry of Health, Illness, and Disease (2009).